Can a Ct Scan Detect Cancer in Lymph Nodes
CT contrast injection and protocols
Robin Smithuis
Radiology department of the Rijnland Hospital in Leiderdorp, the Netherlands
Publicationdate
Optimal contrast enhancement is important for a succesful diagnostic CT-scan.
In this article we will discuss:
- Nuts of contrast enhancement
- Amount of dissimilarity and injection rate
- Timing of CT-serial
- Hash out a few protocols
Basics of contrast-enhancement
Scroll through the phases of enhancement. You tin enlarge the images past clicking on it.
Phases of enhancement
The purpose of contrast-enhanced CT (CECT) is to observe pathology by enhancing the contrast between a lesion and the normal surrounding structures.
Sometimes a lesion volition be hypovascular compared to the normal tissue and in some cases a lesion will be hypervascular to the surrounding tissue in a certain stage of enhancement.
So it is of import to know in which phase a CT should be performed depending on the pathology that y'all are looking for.
Roll through the images to run across the enhancement in the unlike phases.
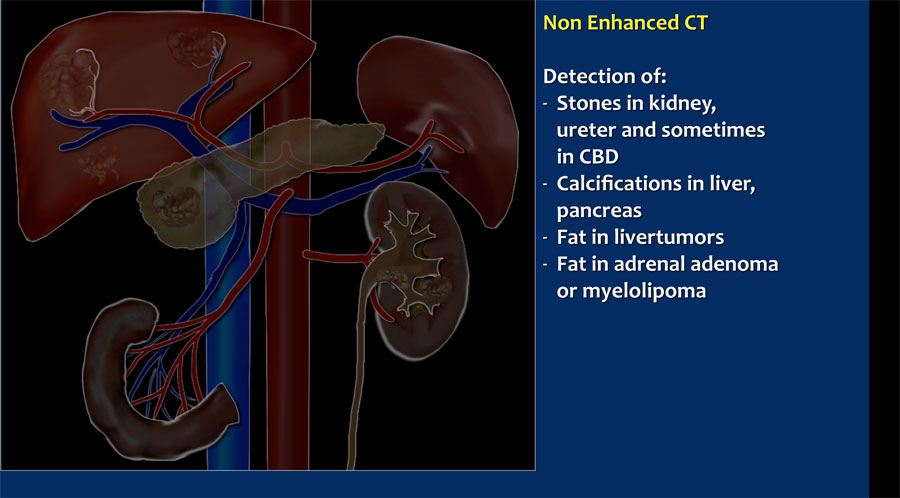
- Non-enhanced CT (NECT)
Helpful in detecting calcifications, fatty in tumors, fatty-stranding as seen in inflammation similar appendicitis, diverticulitis, omental infarction etc. - Early arterial stage - 15-20 sec p.i. or immediately later bolustracking
This is the phase when the contrast is still in the arteries and has non enhanced the organs and other soft tissues. - Late arterial stage - 35-40 sec p.i. or 15-20 sec later on bolustracking. Sometimes also called "arterial phase" or "early venous portal phase", because some enhancement of the portal vein can exist seen. All structures that get their bloodsupply from the arteries will show optimal enhancement.
- Hepatic or late portal stage - lxx-80 sec p.i. or 50-60 sec after bolustracking. Although hepatic phase is the nearly authentic term, most people use the term "belatedly portal phase". In this phase the liver parenchyma enhances through bloodsupply by the portal vein and you should see already some enhancement of the hepatic veins.
- Nephrogenic phase - 100 sec p.i. or 80 sec after bolustracking. This is when all of the renal parenchyma including the medulla enhances. Just in this phase yous will be able to detect small renal cell carcinomas.
- Delayed stage - 6-ten minutes p.i. or half dozen-10 minutes subsequently bolustracking. Sometimes called "wash out phase" or "equilibrium phase". There is launder out of contrast in all abdominal structures except for fibrotic tissue, considering fibrotic tissue has a poor belatedly wash out and will become relatively dense compared to normal tissue. This is comparable to late enhancement of infarcted scar tissue in cardiac MRI.
 Hypervascular lesion is best seen in late arterial stage.
Hypervascular lesion is best seen in late arterial stage.
Timing of CECT
Timing of CT-serial is of import in lodge to grab the right moment of maximal contrast differences between a lesion and the normal parenchyma.
The CT-images show an early arterial phase in comparing to a late arterial stage.
The CT-images are of a patient who underwent ii phases of arterial imaging at 18 and 35 seconds.
In the early arterial phase we nicely meet the arteries, but we simply see some irregular enhancement inside the liver.
In the late arterial stage we can conspicuously identify multiple tumor masses.

You take to adapt your protocol to the blazon of scanner, the speed of dissimilarity injection and to the kind of patient that you lot are examining.
If you have a single slice scanner, it will take near 20 seconds to browse the liver.
For late arterial phase imaging 35 sec is the optimal fourth dimension, and then yous start at virtually 25 seconds and end at about 45 seconds.
Notwithstanding if yous have a 64-slice scanner, you volition be able to examine the whole liver in 4 seconds. So you start scanning at nigh 33 seconds, which is much later.
In aterial phase imaging the time window is narrow, since yous have only limited time before the surrounding liver will start to enhance and obscure a hypervascular lesion.
For Belatedly portal venous phase imaging it is different. Here you don't desire to be likewise early, because you lot want to load the liver with contrast and it takes time for contrast to get from the portal vein into the liver parenchyma. Besides you take more time, because the delayed or equilibrium phase starts at near iii-4 minutes.
Then you lot first at 75 seconds with whatever scanner you have.
Total corporeality of dissimilarity
In many protocols a standard dose is given related to the weight of the patient:
- Weight < 75kg : 100cc
- Weight 75-90kg: 120cc
- Weight > 90kg : 150cc
In some protocols nosotros always want to give the maximum dose of 150cc, like when you are looking for a pancreatic carcinoma or liver metastases.
 Patient with liver cirrhosis and multifocal HCC injected at 2.5ml/sec (left) and at 5ml/sec (right)
Patient with liver cirrhosis and multifocal HCC injected at 2.5ml/sec (left) and at 5ml/sec (right)
Injection charge per unit
5cc/sec through a 18 gauge i.v. catheter
- For all indications, but especially for GI-haemorrhage, livertumor characterisation, pancreatic carcinoma, pulmonary emboli.
- Apply for example a light-green venflon. Exam by fast injection of 10cc NaCl manually.
- Concord the arm stretched.
three-4cc/sec through a 20 guess pink venflon
- If 5cc/sec is not possible or not needed because you are only interested in the tardily portal phase.
The upper images are of a patient with liver cirrhosis and multifocal hepatocellular carcinoma examined after dissimilarity injection at 2.5ml/sec.
Considering of poor enhancement the exam was repeated at 5ml/sec.
At that place is far better dissimilarity enhancement and meliorate tumor detection.

Oral dissimilarity
Some prefer to give positive oral contrast to mark the bowel.
This however has some disadvantages:
- Usually only a portion of the bowel is filled with contrast.
- More than radiation is needed in areas of positive contrast to get the aforementioned quality of images.
- Enhancement of the bowel wall is obscured.
We use fatty containing milk as negative oral contrast or if the patient doesn't drinkable milk nosotros simply use h2o.
Polyethylene glycol (PEG) is also used, and Volumen®, which is a depression density barium suspension.
PEG and Volumen® have the reward that at that place is amend bowel distension.
The CT-prototype shows nice enhancement of the normal bowel wall (xanthous arrows) and no enhancement of the infarcted bowel (red arrows).
This would not be visible if positive oral contrast was given.
Rectal contrast
Rectal contrast is given in cases of suspected bowel perforation or anastomosis leakage.
We use positive contrast: 750 cc water with 50 cc non-ionic water soluable contrast.
More information is given in the protocol anastomosis leakage.
Liver
 Hypervascular tumor (left) enhances in tardily arterial stage. Hypovascular tumor (correct) enhances poorly and is best seen in the hepatic phase
Hypervascular tumor (left) enhances in tardily arterial stage. Hypovascular tumor (correct) enhances poorly and is best seen in the hepatic phase
Dual claret supply
The conspicuity of a liver lesion depends on the attenuation divergence between the lesion and the normal liver.
On a non enhanced CT-scan (NECT) liver tumors are not visible, considering the inherent contrast between tumor tissue and the surrounding liver parenchyma is too low.
When we give i.v. dissimilarity, it is of import to understand, that there is a dual claret supply to the liver.
Normal parenchyma is supplied for 80% by the portal vein and only for 20% by the hepatic artery, so the normal parenchyma will enhance maximally in the hepatic phase at lxx-fourscore sec p.i. and just a piddling flake in the tardily arterial phase at 35-forty sec p.i..
All liver tumors nonetheless get 100% of their blood supply from the hepatic avenue.
Then a hypervascular tumor volition be all-time seen in the late arterial phase.
A hypovascular liver tumor however will enhance poorly in the tardily arterial phase, because it is hypovascular and the surrounding liver does as well enhance poorly in that phase.
This tumor is best seen when the surrounding tissue enhances, i.e. in the late portal (or hepatic) stage at 75-eighty sec p.i.

This figure is to summarize the enhancement patterns.
In the late arterial stage at 35 sec hypervascular lesions similar HCC, FNH, adenoma and hemangioma wil raise optimally, while the normal parenchyma shows simply minimal enhancement.
Hypovascular lesions like metastases, cysts and abscesses will not heighten and are all-time seen in the hepatic phase at 70 sec p.i.
Fibrotic lesions like cholangiocarcinoma and fibrotic metastases hold the contrast much longer than normal parenchyma.
They are best seen in the delayed stage at 600 sec p.i.
This late enhancement is comparable to what is seen in cardiac infarcts in MRI of the heart.

If you want to narrate a liver lesion, you demand maximum contrast at a maximum catamenia rate, i.e. 150cc contrast at 5cc/sec. through a eighteen gauge green venflon.
In about cases you also want to scan the whole abdomen.
You can do this either at 35 sec or 70 sec p.i.
We practise non routinely perform a NECT in gild proceed the radiations dose equally low as possible.
When yous know in advance, that you are dealing with hypovascular metastases, a hepathic phase at seventy sec p.i. is sufficient.
Pancreas
 Pancreatic carcinoma is all-time imaged at 35 sec p.i. Liver metastases are best imaged at 70 sec p.i.
Pancreatic carcinoma is all-time imaged at 35 sec p.i. Liver metastases are best imaged at 70 sec p.i.
Pancreatic carcinoma
Pancreatic carcinoma is a hypovascular tumor and is best detected in the late arterial stage at 35-xl sec p.i. when the normal glandular tissue enhances optimally and the hypovascular tumor does not.
Metastases in the liver are best detected at lxx-80 sec p.i., when the liver parenchyma enhances optimally.
In some cases it tin be difficult to differentiate a pancreatic carcinoma from a focal chronic pancreatitis.
A NECT can be included in the protocol to detect calcifications in the pancreas, just nosotros do not use that in our standard protocol.
Some radiologists apply a longer delay for scanning of the pancreas at 50 sec p.i.

Acute pancreatitis
Imaging in acute pancreatitis is best washed later 72 hours of presentation. read more than...
Ct performed in the first two days can underestimate the severity of the disease.
Necrosis can exist best detected in the late arterial phase at 35 sec p.i.

CT examination of the pancreas should always be done with maximum corporeality of contrast at a maximum flow rate, because both modest pancreatic carcinomas aswell as pancreatic necrosis in pancreatitis are difficult to detect.
It is a matter of personal flavor to practice the whole belly at 35 sec p.i. or at lxx sec p.i.
Some perform ane unmarried CT somewhere inbetween 35 and 70 sec, but that is not what nosotros prefer.
Ileus

Specially in small bowel obstacle (SBO) yous need to reply the near important question: is there strangulation?
To reply that question, you lot need a dissimilarity enhanced CT for the following reasons:
- A scan at 35 sec p.i. is platonic to prove bowel wall enhancement and possible strangulation.
- Sometimes ischemia can exist detected by looking for differences in enhancement of the bowel wall. This is all-time done on coronal thick slabs.
- If there is a closed loop obstruction, this will exist more than obvious on a CECT.
- An obstructing tumor will be better seen.
Do not use positive oral contrast, because this will obscure bowel wall enhancement.

The coronal reconstruction nicely shows bowel wall enhancement in a patient with ileus due to a pocket-size bowel obstruction.
Notice the cluster of thick walled loops with poor enhancement and edema of the mesentery (red circle).
This is a closed loop obstruction with strangulation. This patient needs immediate surgery.
If this patient would have been given positive oral contrast, y'all probably would non have notice the ischemic bowel.
Read more near closed loop obstacle.
Anastomosis leakage

Leakage after bowel surgery is a great clinical problem.
Patients, who are suspected of leakage, need the all-time CT-protocol they tin can get and you equally a radiologist demand the best images to convince the clinician.
You do not desire to tell the surgeon that there is probably leakage, but yous are non certain.
A NECT without whatever oral or rectal dissimilarity is needed to compare with the CECT with rectal contrast, because you don't want to end upward in a word whether some hyperdense stuff outside the bowel is leakage or some post-operative material, dense bowel content or contrast from an earlier examination.
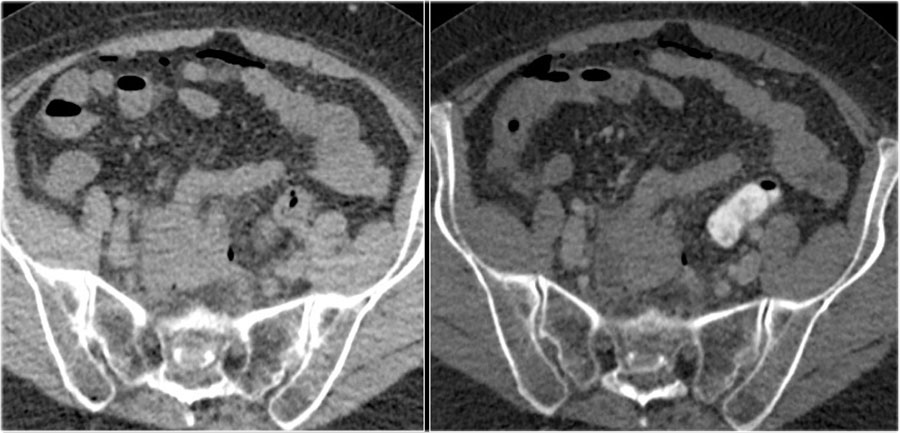
Anastomotic leak. Images on the left prior to rectal contrast and on the correct after rectal contrast.
Here a patient with an anastomosis in the lower abdomen after resection of a sigmoid carcinoma.
Compare the NECT without oral or rectal contrast on the left with the images on the right after rectal contrast.
At that place is no doubt, that dissimilarity in the fluid collection in the right lower abdomen is the upshot of leakage from the bowel (arrow).
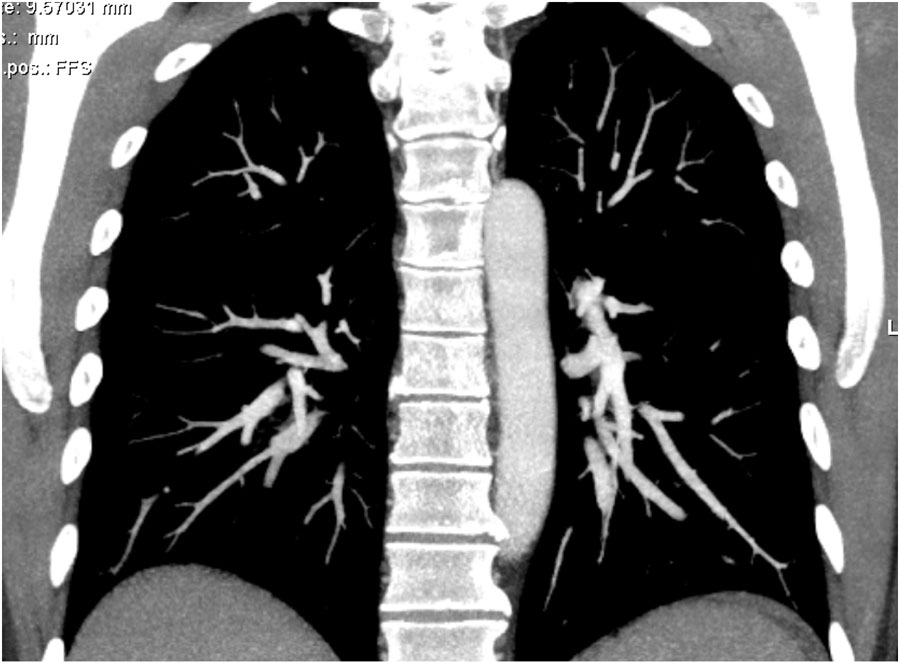
Pulmonary emboli

Skilful quality CT scanning is the nigh important factor for the diagnosis of pulmonary emboli.
On a poor quality scan information technology is impossible to rule out emboli.
We prefer to browse from bottom to top, because if a patient can't hold his breath, so you will have less breathing artefacts in the lower lobes, where most of the emboli are located.
In the upper lobes breathing does not cause that much movement as in the lower parts of the lung.
Nosotros inquire the patient to breath in normally and concur his breath to avoid the transient break of contrast, which will be explained in a moment.

For proficient timing bolus tracking is needed.
A ROI is placed in the pulmonary torso.
When the treshhold of 150 HU is reached, the patient is asked to breath in and scanning is started immediately.
 Transient Suspension of Dissimilarity: Deep inspiration results in dilution of contrast in the right atrium by unopacified claret from the inferior vena cava.
Transient Suspension of Dissimilarity: Deep inspiration results in dilution of contrast in the right atrium by unopacified claret from the inferior vena cava.
Transient pause of contrast
TIC is a menstruation artefact, that consists of relatively poor contrast enhancement in the pulmonary arteries, while there is good enhancement in the SVC and likewise in the aorta, which seems not logic at all.
This vascular phenomenon occurs when the patient performs a deep inspiration simply before the scan starts, resulting in increased venous return of unopacified claret from the inferior vena cava (IVC).
More unopacified blood from the IVC than opacified blood from the SVC enters the correct atrium resulting in poor enhancement of the pulmonary arteries.
This phenomanon is particularly seen in younger patients, who are capable of deep inspiration.
 1. Optimal two. Also late. 3. Transient interruption of contrast
1. Optimal two. Also late. 3. Transient interruption of contrast
The quality of CT depends on skillful contrast commitment and perfect timing.
Scans for pulmonary emboli are frequently of poor quality in young patients and of good quality in old patients.
The explanation is the following:
- Older patients usually have a poor cardiac output, which results in a compact contrast-bolus and good enhancement of the pulmonary vessels (see epitome one).
- Young patients and specially meaning women have a high cardiac output, which results in dilution of the contrast and poor enhancement.
- Young patients are capable of deeper inspiration, which can lead to transient suspension of contrast.
The images demonstrate:
- Optimal enhancement of pulmonary arteries in an sometime patient with a poor cardiac output.
- Poor enhancement of pulmonary arteries due to late scanning.
- Practiced enhancement in SVC and aorta in image 3A, only insufficient enhancement of the pulmonary vessels due to TIC in image 3B.
Scroll through the images.
Thick MIP reconstructions can be helpful in following the vessels and detecting emboli.
Overview of CT-protocols

The tabular array shows an overview of some of the CT-protocols, that we utilise (click to enlarge).
They are based on a 64-piece scanner but can exist used for any CT-scanner independent of manufacturer.
In this tabular array just specific protocols are summarized, since about institutions have their ain standard protocols.
Source: https://radiologyassistant.nl/more/ct-protocols/ct-contrast-injection-and-protocols
Post a Comment for "Can a Ct Scan Detect Cancer in Lymph Nodes"